|
Abstract
Background: Lipoinjection still
has several problems to be resolved; low augmentation
efficiency, fibrosis and calcification, which are derived
from partial necrosis of the injected adipose tissue.
Methods: We have used a disposable screw-type syringe in
order to estimate its usefulness for lipoinjection. In 10
cases, lipoinjection for facial rejuvenation and breast augmentation
was performed using a screw-type syringe with a threaded
plunger and threaded connections for both the connecting
tube and needle to allow precise control and high pressure
injection through an 18-gauge needle.
Results: No postoperative nodules such as fibrosis and calcification
were found clinically and with CT scans, suggesting that
the fat was distributed properly at each site. All patients
were satisfied with the resulting texture, softness, and
absence of foreign materials despite the limited size increase
possible with autologous tissue.
Conclusions: The device was originally made for angiography
and balloon catheter purposes, but we found it very useful
for lipoinjection, especially when a large amount of fat
tissue was to be transplanted.
Introduction
Autologous fat transplantation is one of the promising treatments
for facial rejuvenation and soft-tissue augmentation due
to the lack of incisional scar and complications associated
with foreign materials, though there remain some problems
to be resolved, such as unpredictability and a low survival
rate due to partial necrosis. Lipoinjection can be used for
treating aging hollow face, correcting various kinds of depressed
deformities such as hemifacial microsomia and pectus excavatum,
and is also conducted for breast augmentation in some countries
including Japan, although the use of autologous fat for breast
augmentation is not accepted in other countries including
the United States, which has the highest prevalence of breast
cancer.
The low survival rate of transplanted adipose tissue is the
biggest problem. Many innovations have been reported in an
effort to overcome this problem [1-5] and reviewed previously
[5, 6]. It was concluded that we can harvest fat with a 2.5
mm cannula or 18-gauge needle at -250 to -500 mmHg vacuum
and reinject it with an 18-gauge needle without significant
adipocyte damage [6].
For lipoinjection, the authors used a disposable screw-type
syringe, commercially available in many countries but originally
made for angiography and balloon catheter procedures, and
found it very useful for this purpose, especially when a
large amount of adipose tissue was transplanted. With this
device, lipoaspirates can be injected smoothly through an
18-gauge needle without pre-cutting the harvested tissue,
in precise amounts (e.g. 0.3-1.0 ml each), and easily in
a short time.
Surgical Techniques
Adipose tissue was suctioned with a cannula of 2-mm inner
diameter and a conventional suction machine under general
anesthesia following an infiltration with saline solution
with diluted epinephrine (0.001%). Collected liposuction
tissues were placed in a funnel-shaped 1-liter vessel with
a drain and stopper (liquid separator) (Fig. 1; left, middle),
saline solution was added, and the mixture was left for a
few minutes until good separation was attained. The stopper
was released and the unneeded liquids were drained. This
procedure was repeated 6 or 7 times until the tissues were
almost free of blood and look bright yellow in color (Fig.
1; right).
The washed lipoaspirates were then put into a screw-type
syringe (threaded plunger) with threaded connections for
both the connecting tube and needle to allow for precise
control and high pressure injection through an 18-gauge needle
(Fig. 2; top), and injected into the recipient site of the
body (Fig.2; bottom). This device (10 cc LeVeen? inflator,
Boston Scientific Corp., MA) is originally designed for angiography
and ballon catheter purposes.
For breast augmentation, 200-500 ml lipoaspirates were injected
into each breast with the syringe. To reduce the time of
procedure, two syringes were used; the second syringe was
filled with lipoaspirates prepared for the next injection,
while the first one was used for actual injection. A long
18-gauge needle (60 mm long, Nipro Corp., Tokyo, Japan) was
used for lipoinjection and inserted subcutaneously at several
points around the edge of the breast mound and in the areola
(Fig. 2B). When the long needle was inserted at the edge
of the breast mound, the operator took great care to insert
and place the needle horizontally (parallel to the body line),
in order to avoid damaging the plural and subsequent iatrogenic
pneumothorax. The needle was inserted in various directions,
and was pulled out little by little after each injection
of 0.5-1.0 ml of fat, in order to obtain diffuse distribution
of transplanted fatty tissues (Fig. 3). The fatty tissues
were placed into the fatty layers around and under the mammary
glands, and also carefully into the pectoralis muscles. As
an assistant rotated the plunger according to the operator's
instruction, the operator rigidly held the inserted needle
and pulled it back a short distance after each injection
of a small amount of adipose tissue, The 18-gauge needle
was changed after every 10-20 injections.
For lipoinjection in the face, a short 18-gauge needle was
used instead. If an injection of smaller and more accurate
volume is required, a regular disposable 1cc-syringe may
be used.
Patients
Lipoinjection was performed with this device on a total of
10 patients. In 8 of the cases, adipose tissues were
injected into breasts (220-450 ml on each side), while
the other 2 cases were injected in the face (65-95 ml)
for rejuvenation. Patients' data is summarized in Table
1.
Results
Transplantation of adipose tissue was successfully performed
in all cases, and the time of the injection process ranged
from 55 to 70 min for breast augmentation, and from 15-25
min for facial rejuvenation. Subcutaneous bleeding was usually
seen on some parts of the breasts, and faded away in a week
or so.
Transplanted adipose tissues were gradually absorbed during
the first 3 months, and the contour showed minimal change
thereafter. Representative cases are shown in Figures 4 and
5. In bilateral breast augmentation, the circumference difference
(= chest circumference at the nipple - chest circumference
under the breasts) increased in all cases, usually by 3 to
5 cm. The increase of the circumference difference seems
to correspond to 100-150ml increase in the volume of each
breast mound. All cases showed natural softness of the breasts
without any palpable nodules, and all patients were satisfied
with the resulting texture, softness, and absence of foreign
materials despite the limited size increase possible with
autologous tissue. Postoperatively, no indurations, such
as calcification or fibrosis, were found in any cases, either
clinically or with computed tomography.
Discussion
A number of modifications of lipoinjection techniques have
been tried in order to improve the survival rate of injected
fat. Among those, it is well accepted that adipose tissue
should be transplanted as small particles, preferably within
3 mm in diameter [1]. To perform diffuse distribution of
suctioned fat more efficiently, we have used a disposable
syringe with a threaded plunge and connections.
Though more than half of the grafted fat seemed to be absorbed,
we did not see any indurations such as calcification or fibrosis,
which have been the only factor against the use of lipoinjection
for breast augmentation. No abnormal signs were detected
with postoperative CT scans in our small number of cases.
The results of CT scans showed that transplanted fat tissues
survived and formed a significant thickness of the fatty
layer not only subcutaneously around the mammary glands but
also between the mammary glands and the pectoralis muscles,
indicating successful augmentation of the breast mounds.
Breast volume was nearly settled 6 months after transplatation.
Maximum breast augmentation with this technique appeared
to be 100-150 ml. However, it is a definite advantage that
we do not have to worry about postoperative complications
induced by artificial materials, which include capsular contracture,
hardness, immune response, and breast deformity in the future.
It has been revealed that adipose tissue contains not only
adipogenic progenitor cells but multipotent stem cells which
can differentiate into fat, bone, cartilage, and others [7-10].
Suctioned fat appears to lose a significant amount of these
precursors during mechanical liposuction process compared
to non-suctioned adipose tissue (in preparation), so this
relative deficiency of precursors may contribute to the low
survival rate of transplanted lipoaspirates. It is expected
that a variety of new innovations including stem cell technology
will be further developed and contribute an improved transplanted
fat survival rate fat in the future. Further improvements
of the technique could make fat transfer the first choice
for breast augmentation in the future.
Correspondence to: Kotaro Yoshimura, M. D.
Department of Plastic, Reconstructive, and Aesthetic Surgery,
University of Tokyo,
7-3-1, Hongo, Bunkyo-Ku, Tokyo 113-8655, Japan.
Phone: +81-3-5800-8949
Fax: +81-3-5800-6929
E-mail: yoshimura@cosmetic-medicine.jp
References
1. Carpaneda, C.A., and Ribeiro, M.T. Percentage of graft
viability versus injected volume in adipose autotransplants.
Aesthetic Plast. Surg. 18:17, 1994.
2. Lewis, C.M. Correction of deep gluteal depression by autologous
fat grafting. Aesthetic Plast. Surg. 16: 247, 1992.
3. Ullmann, Y., Hyams, M., Ramon, Y., Peled, I.J., and Leiderbaum,
E.S. Enhancing the survival of aspirated human fat injected
into nude mice. Plast. Reconstr. Surg. 101: 1940, 1998.
4. Har-Shai, Y., Lindenbaum, E.S., Gamliel-Lazarovich, A.,
Beach D., and Hirshowitz, B. An integrated approach for increasing
the survival of autologous fat grafts in the treatment of
contour defects. Plast. Reconstr. Surg. 104: 945, 1999.
5. Ersek, R.A., Chang, P., and Salisbury, M.A. Lipo layering
of autologous fat: an improved technique with promising results.
Plast. Reconstr. Surg. 101: 820, 1998.
6. Shiffman, M.A., and Mirrafati, S. Fat transfer techniques:
the effect of harvest and transfer methods on adipocyte viability
and review of the literature. Dermatol. Surg. 27: 819, 2001.
7. Zuk, P.A., Zhu, M., Mizuno, H., et al. Multilineage cells
from human adipose tissue: implications for cell-based therapies.
Tissue Eng. 7: 211, 2001.
8. Zuk, P.A., Zhu, M., Ashjian, P., et al. Human adipose
tissue is a source of multipotent stem cells. Mol. Biol.
Cell 13: 4279, 2002.
9. Dragoo, J.L., Samimi, B., Zhu, M., et al. Tissue-engineered
cartilage and bone using stem cells from human infrapatellar
fat pads. J. Bone Joint Surg. Br. 85: 740, 2003.
10. Stashower, M., Smith, K., Williams, J., and Skelton,
H. Stromal progenitor cells present within liposuction and
reduction abdominoplasty fat for autologous transfer to aged
skin. Dermatol. Surg. 25: 945, 1999.
Legends

Fig. 1. (left) A funnel-shaped liquid separator with a drain
and stopper. The size of the vessel is about 1-liter.
(middle) Suctioned tissues were poured into the vessel
and kept it in an upright position for a few minutes.
A clear separation between suctioned fat and a liquid
portion were obtained. Note that the liquid portion contained
a significant volume of blood and could be discarded
by opening the clamp. (right) After repeated rinsing
with saline solution, floating fat tissue was cleansed
and looked bright yellow.

Fig. 2. (above) A disposable screw-type syringe with a threaded
plunger (10 cc LeVeen? inflator, Boston Scientific Corp.,
MA). A 60 mm-long 18-gauge needle is connected with a
connection tube, which has threaded connections on both
sides. (below) The device was used for autologous fat
transplantation. The injection needle is rigidly held
by an operator, and a high-pressure injection can be
performed by rotating the plunge by an assistant.
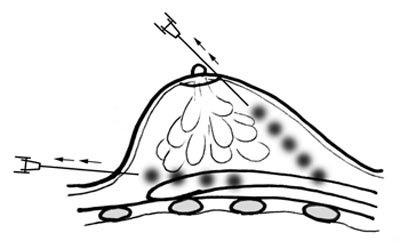
Fig. 3. An injection needle is inserted in variable directions
and planes to complete a diffuse distribution of fatty
tissues. A small amount of fat tissue (0.3-1.0 ml) is
injected to each site as the needle was repeatedly pulled
by a centimeter.

Fig. 4. Case #2 (See Table 1.) (top) A preoperative view.
(middle) A view 6 weeks after surgery; 450 ml of fat
tissue was transplanted into each breast mound. (bottom)
A view at 6 months. Augmented breast mounds were maintained
without leaving any injection scars or subcutaneous indurations.
No more reduction in size was seen thereafter.
Fig. 5. Case #4 (See Table 1).
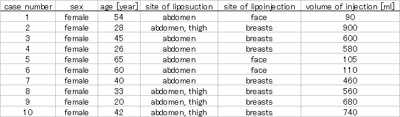
Table 1. Summarized data of cases.
|

