|
Abstract
Background and Objective: Acquired dermal melanocytosis (ADM;
acquired bilateral nevus of Ota-like macules) is known for
its recalcitrance compared to Nevus of Ota, and one of the
reasons seems to be a high rate of post-inflammatory hyperpigmentation
(PIH) after laser treatments.
Methods: Topical bleaching treatment with 0.1% tretinoin
aqueous gel and hydroquinone ointment (4-6 weeks) was initially
performed to discharge epidermal melanin. Subsequently, Q-switched
ruby (QSR) laser was irradiated to eliminate dermal pigmentation.
The both steps were repeated until patients' satisfaction
was obtained. This treatment was performed in 19 patients
with ADM. Skin biopsy was performed in 6 cases at baseline,
after the bleaching pretreatment, and at the end of treatment.
Results: All patients showed good to excellent clearing after
2 to 3 sessions of QSR laser treatments. Total treatment
period ranged from 3 to 13 (mean = 8.3) months. PIH was observed
in 10.5 % of the cases. Histologically, epidermal hyperpigmentation
was observed in all specimens, and was dramatically improved
by the topical bleaching pretreatment.
Conclusion: QSR laser combined with the topical bleaching
pretreatment appeared to consistently treat ADM with low
occurrence rate of PIH and lessen the number of laser sessions
and total treatment period, and may also be applied to any
other lesions with both epidermal and dermal pigmentation.
Introduction
Nevus of Ota, first described by Ota and Tanino as nevus
fuscocaeruleus ophthalmo-maxillaris in 19391, is usually
unilaterally located in the area innervated by the ophthalmic
and maxillary branch of the trigeminal nerve. A typical nevus
of Ota is a flat blue-black or slate-gray macule intermingled
with small, flat, and brown spots. Pigmented macules are
also often present in ocular, oral, and nasal mucous membrane.
On the other hand, acquired bilateral nevus of Ota-like macules
(Hori's nevus) is an acquired pigmented lesion involving
bilateral grayish-brown facial macules that was first reported
by Hori et al. in 19842. This condition and its similar conditions
have been referred to as acquired dermal melanocytosis (ADM)
by some Japanese dermatologists3,4, and we call this condition "ADM" in
this article. ADM onsets later in life most after 20 years
of age, represents bilateral involvements, with the malar
regions almost always affected; and a lack of mucosal and
optic involvement2. It is rare in Caucasians but relatively
common in Asian females, and is seen much more frequently
than nevus of Ota 5. There is a report that it occupied 7.5
% of cosmetic skin complaints in Japan6. Clinically, it can
be easily distinguished from nevus of Ota by bilateral presentation,
spot distribution, and difference in color, whereas, in some
atypical cases, it can be rarely misdiagnosed as melasma.
There are two significant differences in histology between
nevus of Ota and ADM; 1) melanocytes are diffusely distributed
throughout the entire dermis in nevus of Ota, while they
are located only in the upper dermis in ADM, and 2) epidermal
hyperpigmentation is not seen in nevus of Ota, while it is
always prominent in ADM; the latter was not well documented
before, but confirmed in a series of our samples. Difference
in color between nevus of Ota and ADM is due to these histological
differences. Although nevus of Ota responds Q-switched lasers
very well7-11, ADM is known for its recalcitrance to conventional
treatments12-15, and one of the reasons seems to be a high
rate of post-inflammatory hyperpigmentation (PIH) seen after
laser treatments12-14. The authors assumed that it was mainly
due to the presence of epidermal hyperpigmentation and property
of epidermal melanocytes in ADM.
The authors previously described an aggressive and optimal
use of tretinoin along with hydroquinone for various kinds
of skin hyperpigmentation15-17. This topical bleaching treatment
was very effective for removal of epidermal pigmentation.
Therefore, we tried the bleaching pretreatment before Q-switched
ruby (QSR) laser for ADM in order to eliminate epidermal
hyperpigmentation and decrease the risk of PIH after QSR
laser treatment. This combination therapy was applied for
patients with ADM, and its efficacy and usefulness was evaluated.
Patients and Methods
Preparation of Ointments: Tretinoin aqueous gels (tretinoin
gel) at 3 different concentrations (0.1, 0.2, and 0.4 %)
were originally prepared at the Department of Pharmacy, University
of Tokyo, Graduate School of Medicine. The precise regimen
of tretinoin aqueous gel was described before16. An ointment
including 5% hydroquinone and 7% lactic acid (HQ-LA ointment),
and an ointment including 5% hydroquinone and 7% ascorbic
acid (HQ-AA ointment) were also prepared. Plastibase (petrolatum
polyethylene ointment base, Taisho Pharmacology, Osaka, Japan)
was used as the ointment base of the HQ-LA ointment, while
the hydrophilic ointment was used for the HQ-AA ointments.
Because tretinoin gel, HQ-LA, and HQ-AA ointments (especially
tretinoin gel) are pharmacologically unstable, fresh ointments
were prepared at least once a month and stored in a dark
and cool (4oC) place.
Evaluations of results:
Photographs were taken for every patient at baseline and
after treatment with a high-resolution digital camera (Canon
EOS-D30). The percentage of pigmentary clearance was evaluated
via the photographs by two experienced plastic surgeons who
did not perform this treatment. The mean data of the pigmentary
clearance of each patient were classified into 4 categories: "excellent" (80%
or more clearance), "good" (50% to less than 80%
clearance), "fair" (0% to less than 50% clearance),
and "poor" (no change or worse).
Patients: Nineteen Japanese patients with ADM were treated
with our treatment protocol. All patients were women. Patient
age at the start of the treatment ranged from 24 to 50 years
old (37.9 ±8.7; mean ± S.D.). The age of onset of ADM was
15-40 years old (24.7 ±7.5; mean S.D.). Pigmented lesions
were located bilaterally on the malar area in all 19 cases
(100%), on the nose in 4 cases (21%), temporal area in two
cases (11%), and forehead in one case (5%). The follow-up
time after the final laser session ranged from 3 to 13 months
(8.3 ±3.7; mean S.D.).
Treatment Methods: Our treatment was composed of two steps.
The first step was a topical bleaching treatment using tretinoin
gel and hydroquinone ointment (6-8 weeks) and the second
step was QSR laser irradiation. The both steps were repeated
until patients' satisfaction was obtained.
1) Topical bleaching treatment: The purpose of this treatment
is to improve epidermal pigmentation by accelerating discharge
of epidermal melanin (by tretinoin) and suppressing new epidermal
melanogenesis (by hydroquinone). The two-phased (bleaching
and healing) treatment was performed as following.
a) Bleaching phase: 0.1 % tretinoin gel and HQ-LA ointment
were applied initially to the skin lesions twice a day. Tretinoin
gel was carefully applied only on pigmented spots using a
small cotton-tip applicator, while HQ-LA ointment was widely
applied with fingers (e.g. all over the face). The way of
ointment application is critical in this aggressive treatment
in order to obtain maximal bleaching effects with minimal
irritant dermatitis. In case in which severe irritant dermatitis
was induced by HQ-LA ointment, HQ-AA ointment was used instead.
Patients were requested to visit our hospital at 1, 2, 4,
6 and 8 weeks after starting this treatment, and every 4
weeks afterwards. When the appropriate skin reaction (that
is, mild erythema and scaling) was not observed at 1 week,
the concentration of tretinoin was changed to 0.4%. In most
cases, it took 4 to 6 weeks to finish this phase.
b) Healing phase: After 4-6 weeks' bleaching phase, the application
of tretinoin gel and HQ-LA ointment was discontinued, and
application of HQ-AA ointment was used in order to prevent
post-inflammatory hyperpigmentation (PIH) until the redness
was sufficiently reduced. It usually took 2-4 weeks to complete
this phase. Topical corticosteroids were not employed in
either the bleaching or healing phase.
2) QSR laser treatment: In all patients, topical anesthesia
(lidocaine patch; PenlesR, Wyeth Lederle Japan Inc., Tokyo,
Japan) was applied 60-120 minutes before the laser treatment.
For QSR 694.5 nm laser (Model IB101, Niic Co. LTD, Tokyo,
Japan) treatment, spot size of 5 mm, 1 Hz repeat rate, pulse
duration of 20 ns, and fluences ranged from 4.0 to 5.0 J/m2
were used. After laser treatment, topical antibiotics ointment
was applied twice a day until a scale or crust disappeared
(usually for 5-7 days). At 2 weeks after laser treatment,
application of HQ-AA ointment was started.
At 4 weeks after each laser treatment, the topical bleaching
treatment with 0.1% tretinoin gel and HQ-AA ointment was
started as a pretreatment of the next laser irradiation,
and also as a treatment of post-laser PIH in some cases.
In most cases, the bleaching phase for 2 weeks was long enough,
and we can usually estimate the clinical result at 8 weeks
after each laser treatment. When some hyperpigmentation remained,
we can go for the next session. An example of typical time
course was demonstrated in Fig. 1.
Skin biopsy of pigmented regions with a diameter of 2 mm
was performed in 6 cases at baseline, just after the 1st
bleaching treatment, and at the end of the treatment. Sections
were stained with Fontana-Masson staining for visualization
of melanin granules.
Results
Clinical results: In the topical bleaching treatment, erythema
was usually seen in a few days, followed by continual scaling
during the first week. Erythema and scaling were usually
seen continually throughout the bleaching phase. On the other
hand, erythema gradually declined with time in the healing
phase. The difference in color of the macules was usually
observed between before and after the first topical bleaching
treatment; for example, a color change from brown to gray-brown,
or from gray-brown to bluish black, suggesting clearance
of epidermal pigmentation.
All patients showed "good" to "excellent" clearing
after 2 or 3 laser treatments without any complications such
as scarring and persistent depigmentation. Fifteen of 19
cases were evaluated as "excellent" and the other
4 cases as "good" (Table 1). No cases were regarded
as "fine" or "poor". QSR laser treatments
were performed twice in 7 of 19 cases, and 3 times in the
other 12 cases (Table 2). Although PIH apparently occurred
in 2 of 19 cases (10.5 %) after the 1st laser treatment,
PIH was not clearly seen in any cases after the second and
third laser treatments. The average treatment period was
24.8 ± 3.6 (mean ± S.D.) weeks, and the average number of
QSR laser treatment was 2.63 ± 0.5 (mean ± S.D.) times. Although
patients had unpleasing irritant dermatitis during the topical
bleaching treatment, all achieved sufficient satisfaction
with the final results and they were followed up for 8.3
± 3.7 (mean ± S.D.) months (3-13 months) without any evidence
of recurrence. The representative 4 cases are shown in Figs.
2-4.
Histological results: At baseline, not only dermal melanocytosis
but also epidermal melanosis around basal layers was seen
in all 6 samples (Fig. 5). In the upper dermis, elongated,
slender, and pigment-bearing melanocytic cells dispersed
between the collagen fibers were observed. In addition, all
6 specimens showed disappearance of rete ridges. In most
cases, epidermal melanin granules were significantly cleared
after the initial bleaching treatment, while dermal pigmentation
appeared not to change at all (Fig. 6).
Discussion
The first-reported treatment of ADM was cryotherapy19, but
it showed an unpredictable result with a high risk of permanent
scarring and hypopigmentation. Kunachak et al.20 treated
ADM using dermabrasion with successful results. Despite its
advantage as a single session procedure, this approach is
perceived by some patients as an invasive procedure21. Therefore,
QS lasers are considered to be main treatments of ADM today
as well as nevus of Ota.
Although previous reports of QS laser treatments showed good
clearance of ADM12-15,21, it has been pointed out that PIH
and hypopigmentation are frequently observed after the laser
treatments. In ADM, it is known that PIH occurs 2-4 weeks
after laser irradiation in higher degrees and frequency than
in nevus of Ota. Kunachak et al.21 employed repetitive treatment
sessions at only 1-2 weeks intervals. They performed the
second laser session before PIH appeared and reported successful
clearance of ADM but relatively high (5.7 %) risk of hypopigmentation.
Polnikorn et al.12 and Kunachak et al. 14, both used QS Nd:YAG
laser to treat ADM, and reported that the rate of PIH was
71 % and 50 %, respectively. Polnikorn et al.12 waited for
disappearance of PIH before the next session of laser treatment,
and that was 3-6 months. Lam et al.13 used QS alexandrite
laser with the mean session number of 7, and most patients
showed post-laser PIH. In our own experience using QSR laser
for ADM without any pretreatments, PIH was almost always
observed 2-4 weeks after the first laser treatment.
The typical color of ADM is grayish-brown2-4. It is more
brownish than typical nevus of Ota (blue-black, or slate-gray).
The reasons for the difference in color seem to be the existence
of epidermal hyperpigmentation and the location of dermal
melanocytes. In ADM, dermal melanocytes locates more superficial
(the upper dermis2) when compared to nevus of Ota (throughout
the entire dermis22). Although few reports have mentioned
about the epidermal hyperpigmentation of ADM in the past,
we confirmed epidermal hyperpigmentation in all specimens
examined in this study (Fig. 5). We consider that the existence
of epidermal (basal) melanosis is the reason for the difference
in response to laser treatment and incidence rate of PIH
between ADM and nevus of Ota. In addition, all biopsy specimens
showed disappearance of rete ridges, whereas surrounding
intact skin had normal-like rete ridges in some cases. This
finding may clinically mean suppression of epidermal turnover
and discharge of epidermal melanin, and may be related to
the epidermal hyperpigmentation seen in ADM, whereas the
reason for epidermal hyperpigmentation in ADM is unknown
and epidermal melanocytes in ADM are presumably abnormal
like melasma.
In this study, we confirmed histologically that accumulated
melanin granules around the basal layer were cleared up after
treatment with tretinoin and hydroquinone, but the melanin
deposits (dermal melanocytes) in the dermis appeared not
to change in ADM (Fig. 6). Taken together with our previous
studies18,23-25, this finding supports our previous hypothesis
for mechanism of this topical bleaching therapy; Tretinoin
acts as a discharger of epidermal melanin by accelerating
epidermal turnover and promoting keratinocytes proliferation,
while hydroquinone suppresses new melanin production by epidermal
melanocytes.
It is considered that the present combination therapy with
QSR laser and the aggressive bleaching treatment has the
following advantages: 1) High efficiency of the QSR laser
treatment in improving dermal pigmentation; After the pretreatment
removing epidermal pigmentation (basal melanosis), the laser
radiation can be expected to more efficiently get to the
dermis because the laser energy is thought not to be much
absorbed by epidermal melanins 2) Decreasing the rate of
PIH; We assume that, if there is a significant amount of
epidermal pigmentation, considerable inflammation would be
induced in the entire epidermis, resulting in occurrence
of PIH usually 2-4 weeks after laser irradiation. In this
sense, therefore, the pretreatment to discharge epidermal
melanins seems to be quite important. Indeed, with the bleaching
pretreatment, the frequency of PIH after initial laser treatment
was as low as 10.6 %. It was significantly lower than other
studies. In addition, PIH was not clearly detected after
the second or third laser treatment.
Nevus of Ota, which can usually be well treated by several
sessions of QSR laser, have predominantly dermal pigmentation.
This is because, unlike ADM, it does not have significant
epidermal pigmentation, which induces PIH after laser treatments
and makes it more difficult to treat consistently. Therefore,
we prefer the topical bleaching therapy with tretinoin and
hydroquinone for epidermal pigmentation, and QS lasers for
dermal pigmentation, with the exceptions of hyperkeratotic
lesions with such as solar lentigines on extremities and
trunks that we treat with QSR laser. It may be desirable
to perform laser treatments after pretreatment of epidermal
pigmentation for lesions with both epidermal and dermal pigmentation,
such as ADM and hyperpigmentation after atopic dermatitis.
The topical bleaching therapy can treat almost any kinds
of epidermal hyperpigmentation without hyperkeratosis including
PIH and melasma, which can not be treated with lasers.
For treatment of PIH after laser treatments, topical tretinoin
and hydroquinone appeared to be best as we and others13 did,
though the bleaching protocols are not the same. Otherwise,
we can wait for spontaneous clearance of PIH, but the clearance
is not guaranteed and intervals between laser sessions become
much longer such as 3-6 months12. PIH is one of the easiest
pigmented lesions to treat with the topical bleaching treatment17,
and, in this study, a mild treatment with tretinoin for only
2 weeks was usually sufficient, while hydroquinone was used
continually for over 1 month. Even if the pretreatment is
performed, intervals between laser treatments can be shortened
up to 6-8 weeks, therefore leading to shortening the total
treatment period compared with methods waiting for voluntary
disappearance of PIH.
Figures
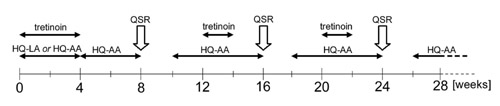
Fig. 1. A representative time
course of the combined treatment. Tretinoin is
used for 4 weeks in the initial bleaching pretreatment,
and for 2 weeks in the following pretreatments.
QSR laser treatment is performed 3 times, and
the total treatment period is 30 weeks.
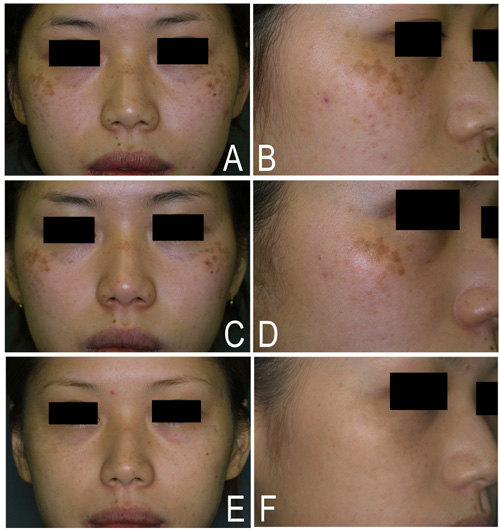
Fig. 2. Case1. A, B) Baseline
photos of a 24-year-old woman with ADM. C, D)
Just after the bleaching treatment with tretinoin
and hydroquinone. The color change of the macules
was moderate, but the histological change was
apparent as shown in Fig. 6. E, F) Six months
after the 3rd QSR laser treatment. Note the complete
clearance of pigmentation.
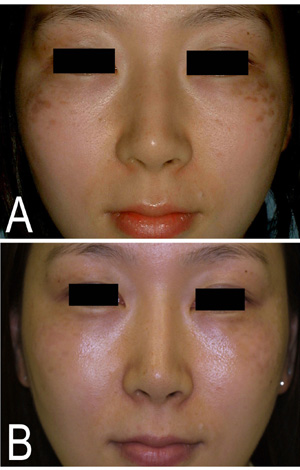
Fig. 3. Case2. A) A baseline view
of a 29-year-old woman with ADM. B) Ten months
after the 3rd QSR laser treatment. The clinical
result was evaluated as "excellent".

Fig. 4. Case3. A) A baseline view
of a 46-year-old woman with ADM. B) Three months
after the 3rd QSR laser treatment. The result
of the clearance was evaluated as "good".
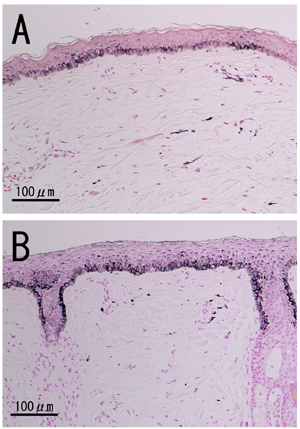
Fig. 5. Histology of ADM before
treatments. Both sections demonstrated epidermal
hyperpigmentation around the basal layer, melanocytosis
in the upper dermis, disappearance of rete ridges,
and slight thinning of the epidermis. (Masson-Fontana
staining; 100X)
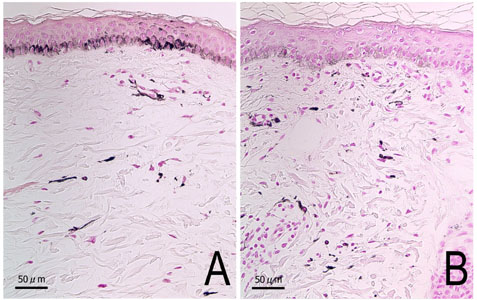
Fig. 6. Histology of ADM in case
1. (A) at baseline, and (B) just after the topical
bleaching pretreatment. A) At baseline, the section
demonstrated epidermal hyperpigmentation as well
as the scattered dermal melanocytes featuring
a highly pigmented, elongated dendritic appearance.
B) Just after the topical bleaching pretreatment,
epidermal pigmentation was significantly improved,
while the dermal menlanocytosis appeared not
to change at all. (Masson-Fontana staining; 200X)
References
1. Ota M, Tanino H. Naevus fuscocaeruleus
ophthalmo-maxillaris and melanosis bulbi. Tokyo
Iji Shinshi 1939;63:1243-5.
2. Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral
nevus of Ota-like macules. J Am Acad Dermatol 1984;10:961-4.
3. Kunachak S, Leelaudomlipi P. Q-switched Nd:YAG laser treatment
for acquired bilateral nevus of ota-like maculae: a long-term
follow-up. Lasers Surg Med 2000;26:376-9.
4. Polnikorn N, Tanrattanakorn S, Goldberg DJ. Treatment
of Hori's nevus with the Q-switched Nd:YAG laser. Dermatol
Surg 2000;26:477-80.
5. Lam AY, Wong DS, Lam LK, et al. A retrospective study
on the efficacy and complications of Q-switched alexandrite
laser in the treatment of acquired bilateral nevus of Ota-like
macules. Dermatol Surg 2001;27:937-41.
6. Kuroki T, Noda H, Ichinose M, et al. Review of patients
with aquired bilateral nevus Ota-like macules. Journal of
Japan Society of Aesthetic Plastic Surgery 1999;21:29-37.
7. Goldberg DJ, Nychay SG. Q-switched ruby laser treatment
of nevus of Ota. J Dermatol Surg Oncol 1992;18:817-21.
8. Geronemus RG. Q-switched ruby laser therapy of nevus of
Ota. Arch Dermatol 1992;128:1618-22.
9. Watanabe S, Takahashi H. Treatment of nevus of Ota with
the Q-switched ruby laser. N Engl J Med 1994;331:1745-50.
10. Alster TS, Williams CM. Treatment of nevus of Ota by
the Q-switched alexandrite laser. Dermatol Surg 1995;21:592-6.
11. Chan HH, Alam M, Kono T, Dover JS. Clinical application
of lasers in Asians. Dermatol Surg 2002;28:556-63.
12. Hidano A. Acquired, bilateral nevus of Ota-like macules.
J Am Acad Dermatol 1985;12:368-9.
13. Sun CC, Lu YC, Lee EF, Nakagawa H. Naevus fusco-caeruleus
zygomaticus. Br J Dermatol 1987;117:545-53.
14. Mizoguchi M, Murakami F, Ito M, et al. Clinical, pathological,
and etiologic aspects of acquired dermal melanocytosis. Pigment
Cell Res 1997;10:176-83.
15. Lee GY, Kim HJ, Whang KK. The effect of combination treatment
of the recalcitrant pigmentary disorders with pigmented laser
and chemical peeling. Dermatol Surg 2002;28:1120-3.
16. Yoshimura K, Harii K, Aoyama T, et al. A new bleaching
protocol for hyperpigmented skin lesions with a high concentration
of all-trans retinoic acid aqueous gel. Aesthetic Plast Surg
1999;23:285-91.
17. Yoshimura K, Harii K, Aoyama T, Iga T. Experience with
a strong bleaching treatment for skin hyperpigmentation in
Orientals. Plast Reconstr Surg 2000;105:1097-108.
18. Yoshimura K, Momosawa A, Watanabe A, et al. Cosmetic
color improvement of the nipple-areola complex by optimal
use of tretinoin and hydroquinone. Dermatol Surg 2002;28:1153-8.
19. Hori Y, Takayama O. Circumscribed dermal melanoses. Classification
and histologic features. Dermatol Clin 1988;6:315-26.
20. Kunachak S, Kunachakr S, Sirikulchayanonta V, Leelaudomniti
P. Dermabrasion is an effective treatment for acquired bilateral
nevus of Ota-like macules. Dermatol Surg 1996;22:559-62.
21. Kunachak S, Leelaudomlipi P, Sirikulchayanonta V. Q-Switched
ruby laser therapy of acquired bilateral nevus of Ota-like
macules. Dermatol Surg 1999;25:938-41.
22. Hirayama T, Suzuki T. A new classification of Ota's nevus
based on histopathological features. Dermatologica 1991;183:169-72.
23. Yoshimura K, Tsukamoto K, Okazaki M, et al. Effects of
all-trans retinoic acid on melanogenesis in pigmented skin
equivalents and monolayer culture of melanocytes. J Dermatol
Sci 2001;27suppl1:68-75.
24. Yoshimura K, Uchida G, Okazaki M, et al. Differential
expression of heparin-binding EGF-like growth factor (HB-EGF)
mRNA in normal human keratinocytes induced by a variety of
natural and synthetic retinoids. Exp Dermatol, in press.
25. Yoshimura K, Momosawa A, Aiba E, et al. Clinical trial
of bleaching treatment with 10 % all-trans retinol gel. Dermatol
Surg, in press.
|