| INTRODUCTION
The use of biodegradable dermal fillers has become
increasingly popular for facial rejuvenation, partly
replacing the conventional surgical procedures with
which long and painful recovery time is unavoidable.1,2
Although numerous kinds of materials have been used
as biodegradable dermal fillers in the last decade2-4,
hyaluronic acid and collagen appear to be the materials
of choice with convincing evidence of their safety
and efficacy2,4-9.
Most common adverse effects of injection of hyaluronic
acid and collagen previously known are bruising and
erythema5,8,10-13. These symptoms almost always resolve
within a week, with no residual complications. The
most serious side effect in the acute phase is localized
tissue necrosis, which is induced by mechanical interruption
of local vascularity and has been reported to occur
very rarely (9 in 10,000 cases who underwent collagen
implantation11). On the other hand, allergic changes,
abscess formation, and granulomatous changes are known
as adverse effects in the chronic phase11,13-15, though
they are less frequent.
Among the adverse effects of dermal fillers, the most
serious one always leading to resultant scar formation
is tissue necrosis. More than half of the reported
cases involved the glabellar region, while only 4%
of them involved the nose11. Only one case of arterial
embolization following the injection of dermal fillers
has been reported16. In this case, the patient underwent
hyaluronic acid injection (RestylaneR) and suffered
transient skin ulceration on the glabella; the ulceration
cured within weeks leaving no cosmetic blemish. Here,
we report a case who received injections of two kinds
of fillers at one time, hyaluronic acid gel (RestylaneR,
Q-Med, Sweden) and human-tissue-derived reconstituted
collagen matrix (ShebaR, Hansbiomed, Korea), and suffered
arterial embolization and distant skin necrosis of
the nasal ala. This is the first detailed report of
nasal alar necrosis associated with arterial embolization
following injection of dermal fillers.
CASE REPORT
A 50-year-old Japanese woman, who had no previous
history of cosmetic surgery, underwent injection of
RestylaneR for shaping the nasal tip contour, and
of ShebaR for wrinkle correction of the upper white
lip and the nasolabial fold and augmentation of the
upper vermillion. Nothing was injected into the nasal
ala. Immediately after the injection the patient had
a striking pain on the left side of the face, and
a few hours later noticed reddish discoloration from
the left side of the nose and the upper lip to the
glabellar region. By the third day from the onset,
blisters appeared at the left nasal ala. When the
patient consulted our hospital on the sixth day, a
gangrenous skin necrosis measuring 1 cm by 1.5 cm
was present on the left nasal ala. (Fig. 1).
Three-dimensional computed tomographic angiography
(3D-CTA) was performed on the 9th day, which suggested
local occlusion of the left angular branch of the
facial artery (Fig. 2). Intravenous administration
of alprostadil (ProstandinR, 120 μg/day) was then
started and the surrounding erythema decreased with
time, but the necrosis extended to the surrounding
skin and subcutaneous tissue, which was surgically
removed on the 12th day (Fig. 3). Histopathological
examination indicated intra-arterial and subdermal
deposition of foreign bodies as well as reactive changes
of the surrounding tissues (Fig. 4). The foreign bodies
were likely the injected dermal fillers, although
we could not identify whether it was Restylane or
Sheba. A full-thickness skin taken from the postauricular
area was grafted to the residual skin defect on the
43rd day, which was successfully accepted.
DISCUSSION
The blood supply of the nasal alar region depends
mainly on the facial artery, of which the running
course and branching are highly varied. Previous studies
demonstrated that the alar region is perfused by two
or three courses of blood supply17-22 (Fig. 5). The
most predominant course is the alar branch of the
facial artery, which branches directly from the angular
branch of the facial artery or from the superior labial
artery. The other courses are communicating arteries
coming through either the nasal dorsum or through
the columella. These arteries are anastomosed with
each other through the subdermal plexus17,18,21.
In the present case, the alar skin resulted in massive
necrosis, despite the absence of filler injection
into the ala. The histopathologic study of the biopsy
specimen of the ala revealed intradermal and intraarterial
foreign bodies (Fig. 4), which showed histopathologic
features comparable to hyaluronic acid or collagen
fillers as previously reported10,11,23,24. Arterial
embolization was suggested also by 3D-CTA that demonstrated
local occlusion of the angular branch of the facial
artery and compensatory dilation of collateral vessels
such as the infraorbital artery and its daughter branches
(Fig. 2). Sharp pain and the erythema observed on
the area nourished by the angular branch of the facial
artery in the early phase also suggested acute and
widespread embolization of the artery. Thus we diagnosed
the patient as suffering from arterial embolizations
of the angular branch and its daughter branches. Theoretically,
accidental injection of filler material into subcutaneous
small vessels caused arterial embolization, developing
into skin necrosis of particular regions.
The only reported case of arterial embolization induced
by hyaluronic acid injection involved the glabellar
region16. In addition, the glabella is the most common
region for local necrosis after bovine collagen injection11.
These cases, however, underwent dermal filler injection
at the same region as subsequent skin necrosis. In
the present case, massive skin necrosis occurred on
the nasal ala, although the patient had no injection
of dermal fillers in the area. Additionally, the patient
had no history of rhinoplasty that would likely affect
the condition of blood supply. Like the glabellar
region, the nasal ala may be a particular region in
which blood supply depends strongly on a single arterial
branch. Otherwise, collateral blood supply through
the nasal tip was blocked by the concurrent filler
injection to the nasal tip, which may be a critical
factor in this case. We could not distinguish whether
the foreign bodies found in the biopsy specimen were
RestylaneR or ShebaR. It also remains unknown whether
physical or biological characteristics of particular
products can influence the susceptibility toward vascular
embolization.
Although biodegradable dermal fillers have been proven
to be sufficiently safe, physicians should recognize
that they are still not devoid of serious side effects
as shown in this case. We think arterial embolization
is an adverse event not only of RestylaneR or ShebaR,
but also of any other dermal filler. The potential
risk of vascular embolization should be noted especially
when treating the nasal alar and perioral regions
as well as the glabellar region. Although accidental
intra-arterial injection of dermal fillers is apparently
rare, fillers should be injected into the dermis,
great care should be taken when injecting into the
subcutis to prevent intra-arterial injection, and
the anatomical feature of the facial artery and its
network should be correctly kept in mind.
REFERENCES
1. de Maio, M. The minimal approach: An innovation
in facial cosmetic procedures. Aesthetic Plast Surg.
28: 295, 2004.
2. Narins, R. S., and Bowman, P. H. Injectable skin
fillers. Clin Plast Surg. 32: 151, 2005.
3. Sclafani, A. P., and Romo, T., 3rd. Injectable
fillers for facial soft tissue enhancement. Facial
Plast Surg. 16: 29, 2000.
4. Homicz, M. R., and Watson, D. Review of injectable
materials for soft tissue augmentation. Facial Plast
Surg. 20: 21, 2004.
5. Bauman, L. Cosmoderm/Cosmoplast (human bioengineered
collagen) for the aging face. Facial Plast Surg. 20:
125, 2004.
6. Narins, R. S., Brandt, F., Leyden, J. et al. A
randomized, double-blind, multicenter comparison of
the efficacy and tolerability of Restylane versus
Zyplast for the correction of nasolabial folds. Dermatol
Surg. 29: 588, 2003.
7. Douglas, R. S., Donsoff, I., Cook, T. et al. Collagen
fillers in facial aesthetic surgery. Facial Plast
Surg. 20: 117, 2004.
8. Friedman, P. M., Mafong, E. A., Kauvar, A. N. et
al. Safety data of injectable nonanimal stabilized
hyaluronic acid gel for soft tissue augmentation.
Dermatol Surg. 28: 491, 2002.
9. Bowman, P. H., and Narins, R. S. Hylans and soft
tissue augmentation. In J. Carruther, A. Carruther,
Procedures in Cosmetic Dermatology Series: Soft Tissue
Augmentation, 1st Ed. Philadelphia: WB Saunders, 2005.
Pp 33-54.
10. Duranti, F., Salti, G., Bovani, B. et al. Injectable
hyaluronic acid gel for soft tissue augmentation.
A clinical and histological study. Dermatol Surg.
24: 1317, 1998.
11. Hanke, C. W., Higley, H. R., Jolivette, D. M.
et al. Abscess formation and local necrosis after
treatment with Zyderm or Zyplast collagen implant.
J Am Acad Dermatol. 25: 319, 1991.
12. Andre, P. Evaluation of the safety of a non-animal
stabilized hyaluronic acid (NASHA -- Q-medical, Sweden)
in european countries: A retrospective study from
1997 to 2001. J Eur Acad Dermatol Venereol. 18: 422,
2004.
13. Lowe, N. J., Maxwell, C. A., Lowe, P. et al. Hyaluronic
acid skin fillers: Adverse reactions and skin testing.
J Am Acad Dermatol. 45: 930, 2001.
14. Lupton, J. R., and Alster, T. S. Cutaneous hypersensitivity
reaction to injectable hyaluronic acid gel. Dermatol
Surg. 26: 135, 2000.
15. Shafir, R., Amir, A., and Gur, E. Long-term complications
of facial injections with Restylane (injectable hyaluronic
acid). Plast Reconstr Surg. 106: 1215, 2000.
16. Schanz, S., Schippert, W., Ulmer, A. et al. Arterial
embolization caused by injection of hyaluronic acid
(Restylane). Br J Dermatol. 146: 928, 2002.
17. Pinar, Y. A., Bilge, O., and Govsa, F. Anatomic
study of the blood supply of perioral region. Clin
Anat. 18: 330, 2005.
18. Jung, D. H., Kim, H. J., Koh, K. S. et al. Arterial
supply of the nasal tip in Asians. Laryngoscope. 110:
308, 2000.
19. Nakajima, H., Imanishi, N., and Aiso, S. Facial
artery in the upper lip and nose: Anatomy and a clinical
application. Plast Reconstr Surg. 109: 855, 2002.
20. Toriumi, D. M., Mueller, R. A., Grosch, T. et
al. Vascular anatomy of the nose and the external
rhinoplasty approach. Arch Otolaryngol Head Neck Surg.
122: 24, 1996.
21. Magden, O., Edizer, M., Atabey, A. et al. Cadaveric
study of the arterial anatomy of the upper lip. Plast
Reconstr Surg. 114: 355, 2004.
22. Rohrich, R. J., Muzaffar, A. R., and Gunter, J.
P. Nasal tip blood supply: Confirming the safety of
the transcolumellar incision in rhinoplasty. Plast
Reconstr Surg. 106: 1640, 2000.
FIGURE LEGENDS
Fig. 1. Views at the
first visit (6 days after injection). Gangrenous skin
necrosis was seen on the left nasal ala. Erythema
was seen on the whole area nourished by the angular
branch of the facial artery; the glabellar region,
the left side of the nose, and the left upper lip.
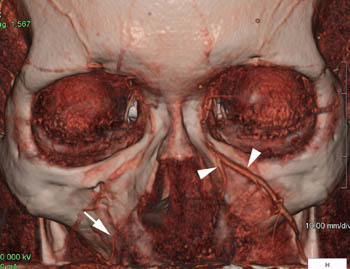
Fig. 2. Three-dimensional computed tomographic angiography
(3D-CTA) on the 9th day. 3D-CTA presented the local
occlusion of the left angular branch of the facial
artery. Compensatory dilation of collateral vessels
from the infraorbital artery was noted (arrowhead).
Contralateral angular branch of the facial artery
was patent and not dilated (arrow).
Fig. 3. Views before
(left), just after (center), and 4 weeks after (right)
debridement of the necrotic skin. Debridement was
performed on the 12th day and skin graft was performed
on 43rd day.
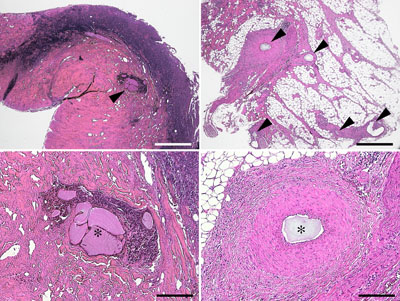
Fig. 4. Histology of debridement sample. Upper left:
low-power photomicrograph of the necrotic skin on
the nasolabial fold shows epidermal necrosis and intradermal
deposition of filler material (arrow). Lower left:
higher magnification of the upper left photograph
shows intradermal foreign bodies (?) accompanied by
infiltration of inflammatory cells. Upper right: low-power
photograph of subcutaneous tissue shows multiple intraarterial
embolizations (arrow). Lower right: higher magnification
ofupper right photograph shows intraarterial foreign
bodies (?) and thickening of the intima. Haematoxylin
and eosin stain. Bar = 800 μm for above and 200 μm
for below.
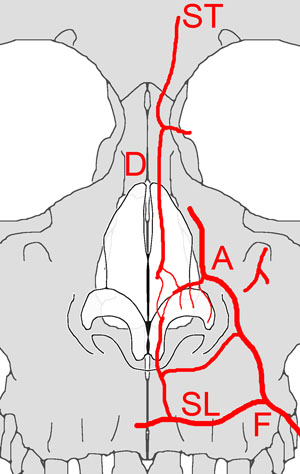
Fig. 5. Schematic view of the blood supply of the
nasal ala. The angular branch (A) of the facial artery
(F) runs along the nasolabial fold, branching off
the superior labial artery (SL). The alar branch is
a terminal branch of the angular branch, which is
the main feeding artery for the nasal ala. The superior
labial artery and the dorsal branch (D) of the superior
trochlear artery (ST) communicate with the alar branch
around the nasal tip.
|